Back and Neck Pain
The
importance of back and neck pain in our society is underscored by the
following: (1) the annual societal cost of back pain in the United States is
estimated to be between $20 and $50 billion; (2) back symptoms are the most
common cause of disability in patients under 45 years of age; (3) 50% of
working adults, in one survey, admitted to having a back injury each year; and
(4) approximately 1% of the U.S. population is chronically disabled because of
back pain.
The
enormous economic pressure to provide rational and efficient care of patients
with back pain has resulted in clinical practice guidelines (CPGs) for these
patients. CPGs are algorithms which guide evaluation or treatment at specific
steps in patient care. CPGs for acute low back pain (ALBP) are based
upon incomplete evidence (see algorithms, Fig. 16-6) but represent an attempt
to standardize common medical practice. Major revisions in CPGs for back pain
can be anticipated in the future. Management of patients with chronic low
back pain (CLBP) is complex and not amenable to a simple algorithmic
approach at this time.
Figure 16-6: Algorithms for management of acute low
back pain, age ![]() 18
years. A. Symptoms <3 months, first 4 weeks. B. Possible
serious etiology.figure-continued1><<016>> C. Management
weeks 4-12. 1
18
years. A. Symptoms <3 months, first 4 weeks. B. Possible
serious etiology.figure-continued1><<016>> C. Management
weeks 4-12. 1![]() ,
entry point from Algorithm D postoperatively or if patient declines surgery. D.
Surgical options. (NSAIDs, nonsteroidal anti-inflammatory drugs; CBC, complete
blood count; ESR, erythrocyte sedimentation rate; UA, urinalysis; EMG,
electromyography; NCV, nerve conduction velocity studies; MRI, magnetic
resonance imaging; CT, computed tomography; CNS, central nervous system.)
,
entry point from Algorithm D postoperatively or if patient declines surgery. D.
Surgical options. (NSAIDs, nonsteroidal anti-inflammatory drugs; CBC, complete
blood count; ESR, erythrocyte sedimentation rate; UA, urinalysis; EMG,
electromyography; NCV, nerve conduction velocity studies; MRI, magnetic
resonance imaging; CT, computed tomography; CNS, central nervous system.)
Anatomy
of the Spine
The
anterior portion of the spine consists of cylindrical vertebral bodies
separated by intervertebral disks and held together by the anterior and
posterior longitudinal ligaments. The intervertebral disks are composed of a
central gelatinous nucleus pulposus surrounded by a tough cartilagenous ring,
the annulus fibrosis; disks are responsible for 25% of spinal column length
(Figs. 16-1 and 16-2). The disks are largest in the cervical and lumbar regions
where movements of the spine are greatest. The disks are elastic in youth and
allow the bony vertebrae to move easily upon each other. Elasticity is lost
with age. The function of the anterior spine is to absorb the shock of typical
body movements such as walking and running.
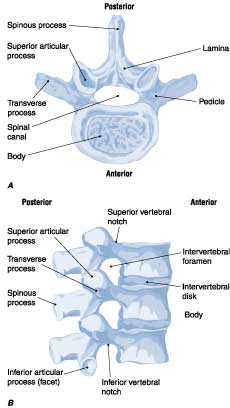
Figure 16-1: Vertebral anatomy.
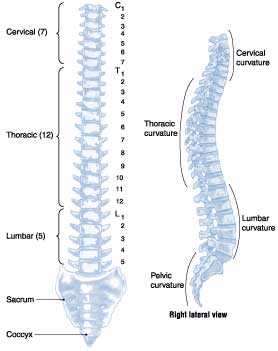
Figure 16-2: Spinal column.
The
posterior portion of the spine consists of the vertebral arches and seven
processes. Each arch consists of paired cylindrical pedicles anteriorly and
paired laminae posteriorly (Fig. 16-1). The vertebral arch gives rise to two
transverse processes laterally, one spinous process posteriorly, plus two
superior and two inferior articular facets. The functions of the posterior
spine are to protect the spinal cord and nerves within the spinal canal and to
stabilize the spine by providing sites for the attachment of muscles and
ligaments. The contraction of muscles attached to the spinous and transverse
processes produces a system of pulleys and levers that results in flexion,
extension, and lateral bending movements of the spine. Normal upright posture
in humans places the center of gravity anterior to the spine. The graded
contraction of well-developed paraspinal muscles attached to the laminae,
transverse processes, and spinous processes is necessary to maintain normal
upright posture.
The
nerve roots exit at a level above their respective vertebral bodies in the
cervical region (the C7 nerve root exits at the C6-C7 level) and below their
respective vertebral bodies in the thoracic and lumbar regions (the T1 nerve
root exits at the T1-T2 level). The spinal cord ends at the L1 or L2 level of
the bony spine. Consequently, the lumbar nerve roots follow a long intraspinal
course and can be injured anywhere from the upper lumbar spine to their exit at
the intervertebral foramen. For example, it is common for disk herniation at
the L4-L5 level to produce compression of the S1 nerve root (Fig. 16-3). In
contrast, cervical nerve roots follow a short intraspinal course and exit at
the level of their respective spinal cord segments (upper cervical) or one
segment below the corresponding levels (lower cervical cord). Cervical spine
pathology can result in spinal cord compression, but lumbar spine pathology
cannot.
Types
of Back Pain
An
understanding of the nature of the pain as described by the patient is the
essential first step in evaluation. Attention is also focused on identification
of risk factors for serious underlying diseases that require specific
evaluation.
Local pain is caused by stretching of pain-sensitive
structures that compress or irritate sensory nerve endings. The site of the
pain is near the affected part of the back.
Pain referred to the back may arise from abdominal or pelvic
viscera. The pain is usually described as primarily abdominal or pelvic but is
accompanied by back pain and usually unaffected by posture. The patient may
occasionally complain of back pain only.
Pain of spine origin may be located in the back or referred to the
buttocks or legs. Diseases affecting the upper lumbar spine tend to refer pain
to the lumbar region, groin, or anterior thighs. Diseases affecting the lower
lumbar spine tend to produce pain referred to the buttocks, posterior thighs,
or rarely the calves or feet. Provocative injections into pain-sensitive
structures of the spine (diskography) may produce leg pain that does not follow
a dermatomal distribution. The exact pathogenesis of this
"sclerotomal" pain is unclear, but it may explain many instances in
which combined back and leg pain is unaccompanied by evidence of nerve root
compression.
Radicular back pain is typically sharp and radiates from the spine
to the leg within the territory of a nerve root (see "Lumbar Disk
Disease," below). Coughing, sneezing, or voluntary contraction of
abdominal muscles (lifting heavy objects or straining at stool) may elicit the
radiating pain. The pain may increase in postures that stretch the nerves and
nerve roots. Sitting stretches the sciatic nerve (L5 and S1 roots) because the nerve
passes posterior to the hip. The femoral nerve (L2, L3, and L4 roots) passes
anterior to the hip and is not stretched by sitting. The description of the
pain alone often fails to distinguish clearly between sclerotomal pain and
radiculopathy.
Pain associated with muscle spasm, although of obscure
origin, is commonly associated with many spine disorders. The spasms are
accompanied by abnormal posture, taut paraspinal muscles, and dull pain.
Back
pain at rest or unassociated with specific postures should raise the index of
suspicion for an underlying serious cause (e.g., spine tumor, fracture,
infection, or referred pain from visceral structures). Knowledge of the
circumstances associated with the onset of back pain is important when weighing
possible serious underlying causes for the pain. Some patients involved in
accidents or work-related injuries may exaggerate their pain for the purpose of
compensation or for psychological reasons.
Examination
of the Back
A
physical examination that includes the abdomen and rectum is advisable. Back
pain referred from visceral organs may be reproduced during palpation of the
abdomen (pancreatitis, abdominal aortic aneurysm) or percussion over the
costovertebral angles (pyelonephritis, adrenal disease, L1-L2 transverse process
fracture).
The
normal spine (Fig. 16-2) displays a thoracic kyphosis, lumbar lordosis, and
cervical lordosis. Exaggeration of these normal alignments may result in
hyperkyphosis (lameback) of the thoracic spine or hyperlordosis (swayback) of
the lumbar spine. Spasm of lumbar paraspinal muscles results in flattening of
the usual lumbar lordosis. Inspection may reveal lateral curvature of the spine
(scoliosis) or an asymmetry in the appearance of the paraspinal muscles,
suggesting muscle spasm. Taut paraspinal muscles limit the motion of the lumbar
spine. Back pain of bony spine origin is often reproduced by palpation or
percussion over the spinous process of the affected vertebrae.
Forward
bending is frequently limited by paraspinal muscle spasm. Flexion of the hips
is normal in patients with lumbar spine disease, but flexion of the lumbar
spine is limited and sometimes painful. Lateral bending to the side opposite
the injured spinal element may stretch the damaged tissues, worsen pain, and
limit motion. Hyperextension of the spine (with the patient prone or standing)
is limited when nerve root compression or bony spine disease is present.
Pain
from hip disease may mimic the pain of lumbar spine disease. The first movement
is typically internal rotation of the hip. Manual internal and external
rotation at the hip with the knee and hip in flexion (Patrick sign) may
reproduce the pain, as may percussion of the heel (of an outstretched leg) with
the palm of the examiner's hand.
In
the supine position passive flexion of the thigh on the abdomen while the knee
is extended produces stretching of the L5 and S1 nerve roots and the sciatic
nerve because the nerve passes posterior to the hip. Passive dorsiflexion of
the foot during the maneuver adds to the stretch. While flexion to at least 80°
is normally possible without causing pain, tight hamstrings commonly limit
motion, may result in pain, and are readily identified by the patient. This straight
leg-raising (SLR) sign is positive if the maneuver reproduces the patient's
usual back or limb pain. Eliciting the SLR sign in the sitting position may
help determine if the finding is reproducible. The patient may describe pain in
the low back, buttocks, posterior thigh, or lower leg, but the key feature is
reproduction of the patient's usual pain. The crossed SLR sign is
positive when performance of the maneuver on one leg reproduces the patient's
pain symptoms in the opposite leg or buttocks. The nerve or nerve root lesion
is always on the side of the pain. The reverse SLR sign is elicited by
standing the patient next to the examination table and passively extending each
leg while the patient continues to stand. This maneuver stretches the L2-L4
nerve roots and the femoral nerve because the nerves pass anterior to the hip.
The reverse SLR test is positive if the maneuver reproduces the patient's usual
back or limb pain.
The
neurologic examination includes a search for weakness, muscle atrophy, focal
reflex changes, diminished sensation in the legs, and signs of spinal cord
injury. Findings with specific nerve root lesions are shown in Table 16-1 and
are discussed below.
Table 16-1: Lumbosacral Radiculopathy-Neurologic
Features
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Laboratory
Studies
Routine
laboratory studies such as a complete blood count, erythrocyte sedimentation
rate, chemistry panel, and urinalysis are rarely needed for the initial
evaluation of acute (<3 months), nonspecific, low back pain. If risk factors
for a serious underlying disease are present, then laboratory studies (guided
by the history and examination) are indicated (Fig. 16-6B).
Plain
films of the lumbar or cervical spine are helpful when risk factors for
vertebral fracture (trauma, chronic steroid use) are present. In the absence
of risk factors, routine x-rays of the lumbar spine in the setting of acute,
nonspecific, low back pain are expensive and rarely helpful. Magnetic
resonance imaging (MRI) and computed tomography (CT)-myelography have emerged
as the radiologic tests of choice for evaluation of most serious diseases
involving the spine. In general, the definition of soft tissue structures by
MRI is superior, whereas CT-myelography provides optimal imaging of bony
lesions in the region of the lateral recess and intervertebral foramen and is
tolerated by claustrophobic patients. With rare exceptions, conventional
myelography and bone scan are inferior to MRI and CT-myelography.
Electromyography
(EMG) can be used to assess the functional integrity of the peripheral nervous
system (Chap. 357) in the setting of back pain. Sensory nerve conduction
studies are normal when focal sensory loss is due to nerve root damage because
the nerve roots are proximal to the nerve cell bodies in the dorsal root
ganglia. The diagnostic yield of needle EMG is higher than that of nerve
conduction studies for radiculopathy. Denervation changes in a myotomal
(segmental) distribution are detected by sampling multiple muscles supplied by
different nerve roots and nerves; the pattern of muscle involvement indicates
the nerve root(s) responsible for the injury. Needle EMG provides objective
information about motor nerve fiber injury when the clinical evaluation of
weakness is limited by pain or poor effort. EMG and nerve conduction studies
will be normal when only limb pain or sensory nerve root injury or irritation
is present. Mixed nerve somatosensory evoked potentials and F-wave studies are
of uncertain value in the evaluation of radiculopathy.
Causes of Back Pain
Congenital Anomalies of the Lumbar Spine
Spondylolysis is a bony defect in the pars interarticularis
(a segment near the junction of the pedicle with the lamina) of the vertebra;
the etiology of the defect may be a stress fracture in a congenitally abnormal
segment. The defect (usually bilateral) is best visualized on oblique
projections in plain x-rays or by CT scan and occurs in the setting of a single
injury, repeated minor injuries, or growth.
Spondylolisthesis is the anterior slippage of the vertebral body,
pedicles, and superior articular facets, leaving the posterior elements behind.
Spondylolisthesis is associated with spondylolysis and degenerative spine
disease and occurs more frequently in women. The slippage may be asymptomatic
but may also cause low back pain, nerve root injury (the L5 root most
frequently), or symptomatic spinal stenosis. Tenderness may be elicited near
the segment that has "slipped" forward (most often L4 on L5 or
occasionally L5 on S1). A "step" may be present on deep palpation of
the posterior elements of the segment above the spondylolisthetic joint. The
trunk may be shortened and the abdomen protuberant as a result of extreme
forward displacement of L4 on L5 in severe degrees of spondylolisthesis. In
these cases, cauda equina syndrome may occur (Chap. 368).
Figure 16-3: Locations of compression of lumbar and
sacral roots by herniated disks.
Pain-sensitive
structures in the spine include the vertebral body periosteum, dura, facet
joints, annulus fibrosus of the intervertebral disk, epidural veins, and the
posterior longitudinal ligament. Damage to these nonneural structures may cause
pain. The nucleus pulposus of the intervertebral disk is not pain-sensitive
under normal circumstances. Pain sensation is conveyed by the sinuvertebral
nerve that arises from the spinal nerve at each spine segment and reenters the
spinal canal through the intervertebral foramen at the same level. Disease of
these diverse pain-sensitive spine structures may explain many cases of back
pain without nerve root compression. The lumbar and cervical spine possess the
greatest potential for movement and injury.
Trauma
Trauma
is an important cause of acute low back pain. A patient complaining of back
pain and inability to move the legs may have a spinal fracture or dislocation,
and, with fractures above L1, spinal cord compression. In such cases care must
be taken to avoid further damage to the spinal cord or nerve roots. The back
should be immobilized pending results of plain x-rays.
Sprains and Strains
The
terms low back sprain, strain, or mechanically induced muscle
spasm are used for minor, self-limited injuries associated with lifting a
heavy object, a fall, or a sudden deceleration such as occurs in an automobile
accident. These terms are used loosely and do not clearly describe a specific
anatomic lesion. The pain is usually confined to the lower back, and there is
no radiation to the buttocks or legs. Patients with low back pain and
paraspinal muscle spasm often assume unusual postures.
Vertebral Fractures
Most
traumatic fractures of the lumbar vertebral bodies result from compression or
flexion injuries producing anterior wedging or compression. With more severe
trauma, the patient may sustain a fracture-dislocation or a "burst"
fracture involving not only the vertebral body but posterior elements as well.
Traumatic vertebral fractures are caused by falls from a height (a pars
interarticularis fracture of the L5 vertebra is common), sudden deceleration in
an automobile accident, or direct injury. Neurologic impairment is commonly
associated with these injuries, and early surgical treatment is indicated
(Chap. 369).
When
fractures are atraumatic, the bone is presumed to be weakened by a pathologic
process. The cause is usually postmenopausal (type 1) or senile (type 2)
osteoporosis (Chap. 342). Underlying systemic disorders such as osteomalacia,
hyperparathyroidism, hyperthyroidism, multiple myeloma, metastatic carcinoma,
or glucocorticoid use may also weaken the vertebral body. The clinical context,
neurologic signs, and x-ray appearance of the spine establish the diagnosis.
Antiresorptive drugs including biphosphatonates, alendronate, transdermal
estrogen, and tamoxifen have been shown to reduce the risk of osteoporotic
fractures.
Lumbar Disk Disease
This
disorder is a common cause of chronic or recurrent low back and leg pain. Disk
disease is most likely to occur at the L4-L5 and L5-S1 levels, but upper lumbar
levels are involved occasionally. The cause of the disk injury is often
unknown; the risk is increased in overweight individuals. Degeneration of the
nucleus pulposus and the annulus fibrosus increases with age and may be
asymptomatic or painful. A sneeze, cough, or trivial movement may cause the
nucleus pulposus to prolapse, pushing the frayed and weakened annulus
posteriorly. In severe disk disease, the nucleus may protrude through the
annulus (herniation) or become extruded to lie as a free fragment in the spinal
canal.
The
mechanism by which intervertebral disk injury causes back pain is
controversial. The inner annulus fibrosus and nucleus pulposis are normally
devoid of innervation. Inflammation and production of proinflammatory cytokines
within the protruding or ruptured disk may trigger or perpetuate back pain. Ingrowth
of nociceptive (pain) nerve fibers into inner portions of diseased
intervertebral disk may be responsible for chronic "diskogenic" pain.
Nerve root injury (radiculopathy) from disk herniation may be due to
compression, inflammation, or both; pathologically, varying degrees of
demyelination and axonal loss are usually present.
The
symptoms of a ruptured intervertebral disk include back pain, abnormal posture,
limitation of spine motion (particularly flexion), or radicular pain. A
dermatomal pattern of sensory loss or a reduction in or loss of a deep tendon
reflex is more suggestive of a specific root lesion than the pattern of pain.
Motor findings (focal weakness, muscle atrophy, or fasciculations) occur less
frequently than sensory or reflex changes, but a myotomal pattern of
involvement can suggest specific nerve root injury. Lumbar disk disease is
usually unilateral (Fig. 16-4), but bilateral involvement does occur with large
central disk herniations that compress several nerve roots at the same level. Clinical
manifestations of specific lumbosacral nerve root lesions are summarized in
Table 16-1. There is evidence to suggest that lumbar disk herniation with a
nonprogressive nerve root deficit can be managed conservatively (i.e.,
nonsurgically) with a successful outcome. The size of the disk protrusion may
naturally decrease over time.
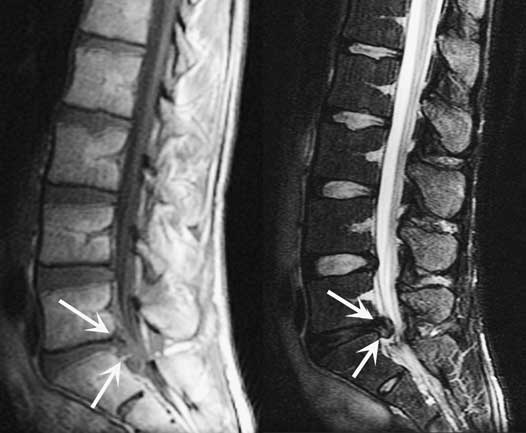
Figure 16-4: Lumbar herniated disk; left S1 radiculopathy.
Sagittal T1-weighted image on the left with arrows outlining disk margins.
Sagittal T2 image on the right reveals a protruding disk at the L5-S1 level (arrows),
which displaces the central thecal sac.
Degeneration
of the intervertebral disk without frank extrusion of disk tissue may give rise
to low back pain only. There may be referred pain in the leg, buttock, or hip
with little or no discomfort in the back and no signs of nerve root
involvement. Lumbar disk syndromes are usually unilateral, but large central
disk herniations can cause bilateral symptoms and signs and may produce a cauda
equina syndrome.
Breakaway
weakness describes a variable power of muscle contraction by a patient who is
asked to provide maximal effort. The weakness may be due to pain or a
combination of pain and underlying true weakness. Breakaway weakness without
pain is due to lack of effort; patients who exhibit breakaway weakness should
be asked if testing a specific muscle is painful. In uncertain cases, EMG can
determine whether or not true weakness is present.
The
differential diagnosis of lumbar disk disease includes a variety of serious and
treatable conditions, including epidural abscess, hematoma, or tumor. Fever,
constant pain uninfluenced by position, sphincter abnormalities, or signs of
spinal cord disease suggest an etiology other than lumbar disk disease.
Bilateral absence of ankle reflexes can be a normal finding in old age or a
sign of bilateral S1 radiculopathy. An absent deep tendon reflex or focal
sensory loss may reflect injury to a nerve root, but other sites of injury
along the nerve must also be considered. For example, an absent knee reflex may
be due to a femoral neuropathy rather than an L4 nerve root injury. A focal
decrease in sensation over the foot and distal lateral calf may result from a
peroneal or lateral sciatic neuropathy rather than an L5 nerve root injury.
Focal muscle atrophy may reflect loss of motor axons from a nerve root or
peripheral nerve injury, an anterior horn cell disease, or disuse.
An
MRI scan or CT-myelogram is necessary to establish the location and type of
pathology. Simple MRI yields exquisite views of intraspinal and adjacent soft
tissue anatomy and is more likely to establish a specific anatomic diagnosis
than plain films or myelography. Bony lesions of the lateral recess or
intervertebral foramen may be seen with optimal clarity on CT-myelographic
studies.
The
correlation of neuroradiologic findings to symptoms, particularly pain, is
often problematic. As examples, contrast-enhancing tears in the annulus
fibrosus or disk protrusions are widely accepted as common sources of back
pain. However, one recent study found that over half of asymptomatic adults
have annular tears on lumbar spine MR imaging, nearly all of which demonstrate
contrast enhancement. Furthermore, asymptomatic disk protrusions are common in
adults, and many of these abnormalities enhance with contrast. These
observations strongly suggest that MRI findings of disk protrusion, tears in
the annulus fibrosus, or contrast enhancement are common incidental findings
that by themselves should not dictate management decisions for patients with
back pain. The presence or absence of persistent disk herniation 10 years after
surgical or conservative treatment has no bearing on a successful clinical
outcome.
There
are four indications for intervertebral disk surgery: (1) progressive motor
weakness from nerve root injury demonstrated on clinical examination or EMG,
(2) bowel or bladder disturbance or other signs of spinal cord disease, (3)
incapacitating nerve root pain despite conservative treatment for at least 4
weeks, and (4) recurrent incapacitating pain despite conservative treatment.
The latter two criteria are more subjective and less well established than the
others. Surgical treatment should also be considered if the pain and/or
neurologic findings do not substantially improve over 4 to 12 weeks.
Surgery
is preceded by MRI scan or CT-myelogram to define the location and type of
pathology. The usual surgical procedure is a partial hemilaminectomy with
excision of the involved and prolapsed intervertebral disk. Arthrodesis of the
involved lumbar segments is considered only in the presence of significant
spinal instability (i.e., degenerative spondylolisthesis or isthmic
spondylolysis).
Other Causes of Low Back Pain
Spinal stenosis is an anatomic diagnosis reflecting a narrowed
lumbar or cervical spinal canal. Classic neurogenic claudication occurs
in the setting of moderate to severe spinal stenosis and typically consists of
back and buttock or leg pain induced by walking or standing. The pain is
relieved by sitting. Symptoms in the legs are usually bilateral. Focal
weakness, sensory loss, or reflex changes may occur when associated with
radiculopathy. Unlike vascular claudication, the symptoms are often provoked by
standing without walking. Unlike lumbar disk disease, the symptoms are usually
relieved by sitting. Severe neurologic deficits, including paralysis and
urinary incontinence, occur rarely. Spinal stenosis usually results from
acquired (75%), congenital, or mixed acquired/congenital factors. Congenital
forms (achondroplasia, idiopathic) are characterized by short, thick pedicles
that produce both spinal canal and lateral recess stenosis. Acquired factors
that may contribute to spinal stenosis include degenerative diseases
(spondylosis, spondylolisthesis, scoliosis), trauma, spine surgery
(postlaminectomy, fusion), metabolic or endocrine disorders (epidural
lipomatosis, osteoporosis, acromegaly, renal osteodystrophy,
hypoparathyroidism), and Paget's disease. MRI or CT-myelography provide the
best definition of the abnormal anatomy (Fig. 16-5).

Figure 16-5: Spinal stenosis. Sagittal T2 fast spin
echo magnetic resonance imaging of a normal (left) and stenotic (right) lumbar
spine, revealing multifocal narrowing (arrows) of the cerebrospinal fluid
spaces surrounding the nerve roots within the thecal sac.
Conservative
treatment includes nonsteroidal anti-inflammatory drugs (NSAIDs), exercise
programs, and symptomatic treatment of acute pain exacerbations. Surgical
therapy is considered when medical therapy does not relieve pain sufficiently
to allow for activities of daily living or when significant focal neurologic
signs are present. Between 65 and 80% of properly selected patients treated
surgically experience >75% relief of back and leg pain. Up to 25% develop
recurrent stenosis at the same spinal level or an adjacent level 5 years after
the initial surgery; recurrent symptoms usually respond to a second surgical
decompression.
Facet joint hypertrophy can produce unilateral radicular
symptoms, due to bony compression, that are indistinguishable from disk-related
radiculopathy. Patients may exhibit stretch signs, focal motor weakness,
hyporeflexia, or sensory loss. Hypertrophic superior or inferior facets can
often be visualized radiologically. Foraminotomy results in long-term relief of
leg and back pain in 80 to 90% of patients.
Lumbar adhesive arachnoiditis with radiculopathy is
the result of a fibrotic process following an inflammatory response to local
tissue injury within the subarachnoid space. The fibrosis results in nerve root
adhesions, producing back and leg pain associated with motor, sensory, and
reflex changes. Myelography-induced arachnoiditis has become rare with the
abandonment of oil-based contrast. Other causes of arachnoiditis include
multiple lumbar operations, chronic spinal infections, spinal cord injury,
intrathecal hemorrhage, intrathecal injection of steroids and anesthetics, and
foreign bodies. The spine MRI appearance of arachnoiditis includes nerve roots
clumping together centrally and adherent to the dura peripherally, or loculations
of cerebrospinal fluid (CSF) within the thecal sac that obscure nerve root
visualization. Treatment is often unsatisfactory. Microsurgical lysis of
adhesions, dorsal rhizotomy, and dorsal root ganglionectomy have resulted in
poor outcomes. Dorsal column stimulation for pain relief has produced varying
results. Epidural steroid injections have been of limited value.
Arthritis
Arthritis
is a major cause of spine pain.
Spondylosis
Osteoarthritic
spine disease typically occurs in later life and primarily involves the
cervical and lumbosacral spine. Patients often complain of back pain that is
increased by motion and associated with stiffness or limitation of motion. The
relationship between clinical symptoms and radiologic findings is usually not straightforward.
Pain may be prominent when x-ray findings are minimal; alternatively, large
osteophytes can be seen in asymptomatic patients in middle and later life.
Hypertrophied facets and osteophytes may compress nerve roots in the lateral
recess or intervertebral foramen. Osteophytes arising from the vertebral body
may cause or contribute to central spinal canal stenosis. Loss of
intervertebral disk height reduces the vertical dimensions of the
intervertebral foramen; the descending pedicle may compress the nerve root
exiting at that level. Osteoarthritic changes in the lumbar spine may rarely
compress the cauda equina.
Ankylosing Spondylitis
This
distinctive arthritic spine disease typically presents with the insidious onset
of low back and buttock pain. Patients are often males below age 40. Associated
features include morning back stiffness, nocturnal pain, pain unrelieved by
rest, an elevated sedimentation rate, and the histocompatibility antigen
HLA-B27. The differential diagnosis includes tumor and infection. Onset at a
young age and back pain characteristically improving with exercise suggest
ankylosing spondylitis. Loss of the normal lumbar lordosis and exaggeration of
thoracic kyphosis are seen as the disease progresses. Inflammation and erosion
of the outer fibers of the annulus fibrosus at the point of contact with the
vertebral body are followed by ossification and bone growth. Bony growth
(syndesmophyte) bridges adjacent vertebral bodies and results in reduced spine
mobility in all planes. The radiologic hallmarks of the disease are
periarticular destructive changes, sclerosis of the sacroiliac joints, and
bridging of vertebral bodies by bone to produce the fused "bamboo
spine." Similar restricted movement may accompany Reiter's syndrome,
psoriatic arthritis, and chronic inflammatory bowel disease. Stress fractures
through the spontaneously ankylosed posterior bony elements of the rigid,
osteoporotic spine may result in focal spine pain, spinal cord compression or
cauda equina syndrome. Occasional atlantoaxial subluxation with spinal cord
compression occurs. Bilateral ankylosis of the ribs to the spine and a decrease
in the height of axial thoracic structures may cause marked impairment of
respiratory function.
Other Destructive Diseases
Neoplasm
Back
pain is the most common neurologic symptom among patients with systemic cancer.
One-third of patients with undiagnosed back or neck pain and known systemic
cancer have epidural extension or metastasis of tumor, and one-third have pain
associated with vertebral metastases alone. About 11% have back pain unrelated
to metastatic disease. Metastatic carcinoma (breast, lung, prostate, thyroid,
kidney, gastrointestinal tract), multiple myeloma, and non-Hodgkin's and
Hodgkin's lymphomas frequently involve the spine. Back pain may be the
presenting symptom because the primary tumor site may be overlooked or
asymptomatic. The pain tends to be constant, dull, unrelieved by rest, and
worse at night. In contrast, mechanical low back pain is usually improved with
rest. Plain x-rays usually, though not always, show destructive lesions in one
or several vertebral bodies without disk space involvement. MRI or
CT-myelography are the studies of choice in the setting of suspected spinal
metastasis, but the trend of evidence favors the use of MRI. The procedure of
choice is the study most rapidly available because the patient may worsen
during a diagnostic delay.
Infection
Vertebral osteomyelitis is usually caused by staphylococci, but
other bacteria or the tubercle bacillus (Pott's disease) may be the responsible
organism. A primary source of infection, most often from the urinary tract,
skin, or lungs, can be identified in 40% of patients. Intravenous drug use is a
well-recognized risk factor. Back pain exacerbated by motion and unrelieved by
rest, spine tenderness over the involved spine segment, and an elevated
erythrocyte sedimentation rate are the most common findings. Fever or elevated
white blood cell count are found in a minority of patients. Plain radiographs
may show a narrowed disk space with erosion of adjacent vertebrae; these
diagnostic changes may take weeks or months to appear. MRI and CT are sensitive
and specific for osteomyelitis; MRI definition of soft tissue detail is
exquisite. CT scan may be more readily available and better tolerated by some
patients with severe back pain.
Spinal epidural abscess (Chap. 368) presents with back pain
(aggravated by palpation or movement) and fever. The patient may exhibit nerve
root injury or spinal cord compression accompanied by a sensory level,
incontinence, or paraplegia. The abscess may track over multiple spinal levels
and is best delineated by spine MRI.
Osteoporosis and Osteosclerosis
Considerable
loss of bone may occur with or without symptoms in association with medical
disorders, including hyperparathyroidism, chronic glucocorticoid use, or
immobilization. Compression fractures occur in up to half of patients with
severe osteoporosis. The risk of osteoporotic vertebral fracture is 4.5 times
greater over 3 years among patients with a baseline fracture compared with
osteoporotic controls. The sole manifestation of a compression fracture may be
focal lumbar or thoracic aching (often after a trivial injury) that is
exacerbated by movement. Other patients experience thoracic or upper lumbar
radicular pain. Focal spine tenderness is common. When compression fractures
are found, treatable risk factors should be sought. Compression fractures above
the midthoracic region suggest malignancy.
Osteosclerosis
is readily identifiable on routine x-ray studies (e.g., Paget's disease) and
may or may not produce back pain. Spinal cord or nerve root compression may
result from bony encroachment on the spinal canal or intervertebral foramina.
Single dual-beam photon absorptiometry or quantitative CT can be used to detect
small changes in bone mineral density. For further discussion of these bone
disorders, see Chaps. 341 to 343.
Referred Pain from Visceral Disease
Diseases
of the pelvis, abdomen, or thorax may produce referred pain to the posterior
portion of the spinal segment that innervates the diseased organ. Occasionally,
back pain may be the first and only sign. In general, pelvic diseases refer
pain to the sacral region, lower abdominal diseases to the lumbar region
(around the second to fourth lumbar vertebrae), and upper abdominal diseases to
the lower thoracic or upper lumbar region (eighth thoracic to the first and
second lumbar vertebrae). Local signs (pain with spine palpation, paraspinal
muscle spasm) are absent, and minimal or no pain accompanies normal spine
movements.
Low Thoracic and Upper Lumbar Pain in Abdominal
Disease
Peptic
ulcer or tumor of the posterior stomach or duodenum typically produces
epigastric pain (Chaps. 285 and 90), but midline back or paraspinal pain may
occur if retroperitoneal extension is present. Back pain due to peptic ulcer
may be precipitated by ingestion of an orange, alcohol, or coffee and relieved
by food or antacids. Fatty foods are more likely to induce back pain associated
with biliary disease. Diseases of the pancreas may produce back pain to the
right of the spine (head of the pancreas involved) or to the left (body or tail
involved). Pathology in retroperitoneal structures (hemorrhage, tumors,
pyelonephritis) may produce paraspinal pain with radiation to the lower
abdomen, groin, or anterior thighs. A mass in the iliopsoas region often
produces unilateral lumbar pain with radiation toward the groin, labia, or
testicle. The sudden appearance of lumbar pain in a patient receiving anticoagulants
suggests retroperitoneal hemorrhage.
Isolated
low back pain occurs in 15 to 20% of patients with a contained rupture of an
abdominal aortic aneurysm (AAA). The classic clinical triad of abdominal pain,
shock, and back pain in an elderly man occurs in fewer than 20% of patients.
Two of these three features are present in two-thirds of patients, and
hypotension is present in half. Ruptured AAA has a high mortality rate; the
typical patient is an elderly male smoker with back pain. The diagnosis is initially
missed in at least one-third of patients because the symptoms and signs can be
nonspecific. Common misdiagnoses include nonspecific back pain, diverticulitis,
renal colic, sepsis, and myocardial infarction. A careful abdominal examination
revealing a pulsatile mass (present in 50 to 75% of patients) is an important
physical finding.
Lumbar Pain with Lower Abdominal Diseases
Inflammatory
bowel disorders (colitis, diverticulitis) or colonic neoplasms may produce
lower abdominal pain, midlumbar back pain, or both. The pain may have a
beltlike distribution around the body. A lesion in the transverse or initial
descending colon may refer pain to the middle or left back at the L2-L3 level.
Sigmoid colon disease may refer pain to the upper sacral or midline suprapubic
regions or left lower quadrant of the abdomen.
Sacral Pain in Gynecologic and Urologic Disease
Pelvic
organs rarely cause low back pain, except for gynecologic disorders involving
the uterosacral ligaments. The pain is referred to the sacral region.
Endometriosis or uterine carcinoma may invade the uterosacral ligaments;
malposition of the uterus may cause uterosacral ligament traction. The pain
associated with endometriosis begins during the premenstrual phase and often
continues until it merges with menstrual pain. Malposition of the uterus
(retroversion, descensus, and prolapse) may lead to sacral pain after standing
for several hours.
Menstrual
pain may be felt in the sacral region. The poorly localized, cramping pain can
radiate down the legs. Other pelvic sources of low back pain include neoplastic
invasion of pelvic nerves, radiation necrosis, and pregnancy. Pain due to
neoplastic infiltration of nerves is typically continuous, progressive in
severity, and unrelieved by rest at night. Radiation therapy of pelvic tumors
may produce sacral pain from late radiation necrosis of tissue or nerves. Low
back pain with radiation into one or both thighs is common in the last weeks of
pregnancy.
Urologic
sources of lumbosacral back pain include chronic prostatitis, prostate
carcinoma with spinal metastasis, and diseases of the kidney and ureter.
Lesions of the bladder and testes do not usually produce back pain. The
diagnosis of metastatic prostate carcinoma is established by rectal
examination, spine imaging studies (MRI or CT), and measurement of
prostate-specific antigen (PSA) (Chap. 95). Infectious, inflammatory, or
neoplastic renal diseases may result in ipsilateral lumbosacral pain, as can
renal artery or vein thrombosis. Ureteral obstruction due to renal stones may
produce paraspinal lumbar pain.
Postural Back Pain
There
is a group of patients with chronic, nonspecific low back pain in whom no
anatomic or pathologic lesion can be found despite exhaustive investigation.
These individuals complain of vague, diffuse back pain with prolonged sitting
or standing that is relieved by rest. The physical examination is unrevealing
except for "poor posture." Imaging studies and laboratory evaluations
are normal. Exercises to strengthen the paraspinal and abdominal muscles are
sometimes therapeutic.
Psychiatric Disease
Chronic
low back pain (CLBP) may be encountered in patients with compensation hysteria,
malingering, substance abuse, chronic anxiety states, or depression. Many
patients with CLBP have a history of psychiatric illness (depression, anxiety,
substance abuse) or childhood trauma (physical or sexual abuse) that antedates
the onset of back pain. Preoperative psychological assessment has been used to
exclude patients with marked psychological impairment who are at high risk for
a poor surgical outcome. It is important to be certain that the back pain in
these patients does not represent serious spine or visceral pathology in
addition to the impaired psychological state.
Unidentified
The
cause of low back pain occasionally remains unclear. Some patients have had
multiple operations for disk disease but have persistent pain and disability.
The original indications for surgery may have been questionable with back pain
only, no definite neurologic signs, or a minor disk bulge noted on CT or MRI.
Scoring systems based upon neurologic signs, psychological factors, physiologic
studies, and imaging studies have been devised to minimize the likelihood of
unsuccessful surgical explorations and to avoid selection of patients with
psychological profiles that predict poor functional outcomes.
![]() Treatment
Treatment
Acute Low Back Pain
A
practical approach to the management of low back pain is to consider acute and
chronic presentations separately. ALBP is defined as pain of less than 3
months' duration. Full recovery can be expected in 85% of adults with ALBP
unaccompanied by leg pain. Most of these patients exhibit "mechanical"
symptoms-pain that is aggravated by motion and relieved by rest.
Observational,
population-based studies have been used to justify a minimalist approach to
individual patient care. These studies share a number of limitations: (1) a
true placebo control group is often lacking; (2) patients who consult different
provider groups (generalists, orthopedists, neurologists) are assumed to have
similar etiologies for their back pain; (3) no information is provided about
the details of treatment within each provider group or between provider groups;
and (4) no attempt to tabulate serious causes of ALBP is made. The
appropriateness of specific diagnostic procedures or therapeutic interventions
for low back pain cannot be assessed from these studies.
The
proposed algorithms (Fig. 16-6) for management of ALBP in adults draw
considerably from published guidelines. However, it must be emphasized that
current CPGs for the treatment of low back pain are based on incomplete
evidence-for example, there is a paucity of well-designed studies documenting
the natural history of disk lesions associated with a focal neurologic deficit.
Guidelines should not substitute for sound clinical judgment.
The
initial assessment excludes serious causes of spine pathology that require
urgent intervention, including infection, cancer, and trauma. Risks factors for
a possible serious underlying cause of back pain include: age > 50 years,
prior diagnosis of cancer or other serious medical illness, bed rest without
relief, duration of pain >1 month, urinary incontinence or recent nocturia,
focal leg weakness or numbness, pain radiating into the leg(s) from the back,
intravenous drug use, chronic infection (pulmonary or urinary), pain increasing
with standing and relieved by sitting, history of spine trauma, and
glucocorticoid use. Clinical signs associated with a possible serious etiology
include unexplained fever, well-documented and unexplained weight loss,
positive SLR sign or reverse SLR sign, crossed SLR sign, percussion tenderness
over the spine or costovertebral angle, an abdominal mass (pulsatile or
nonpulsatile), a rectal mass, focal sensory loss (saddle anesthesia or focal
limb sensory loss), true leg weakness, spasticity, and asymmetric leg reflexes.
Laboratory studies are unnecessary unless a serious underlying cause (Fig.
16-6, Algorithms A and B) is suspected. Plain spine films are
rarely indicated in the first month of symptoms unless a spine fracture is
suspected.
The
roles of bed rest, early exercise, and traction in the treatment of acute
uncomplicated low back pain have been the subject of recent prospective
studies. Clinical trials fail to demonstrate any benefit of prolonged (>2
days) bed rest for ALBP. There is evidence that bed rest is also ineffective
for patients with sciatica or for acute back pain with findings of nerve root
injury. Theoretical advantages of early ambulation for ALBP include maintenance
of cardiovascular conditioning, improved disk and cartilage nutrition, improved
bone and muscle strength, and increased endorphin levels. A recent trial did
not show benefit from an early vigorous exercise program, but the benefits of
less vigorous exercise or other exercise programs remain unknown. The early
resumption of normal physical activity (without heavy manual labor) is likely
to be beneficial. Well-designed clinical studies of traction that include a
sham traction group have failed to show a benefit of traction for ALBP. Despite
this knowledge, one survey of physicians' perceptions of effective treatment
identified strict bed rest for >3 days, trigger point injections (see
below), and physical therapy (PT) as beneficial for more than 50% of patients
with ALBP. In many instances, the behavior of treating physicians does not
reflect the current medical literature.
Proof
is lacking to support the treatment of acute back and neck pain with
acupuncture, transcutaneous electrical nerve stimulation, massage, ultrasound,
diathermy, or electrical stimulation. Cervical collars can be modestly helpful
by limiting spontaneous and reflex neck movements that exacerbate pain.
Evidence regarding the efficacy of ice or heat is lacking, but these
interventions are optional given the lack of negative evidence, low cost, and
low risk. Biofeedback has not been studied rigorously. Facet joint, trigger
point, and ligament injections are not recommended in the treatment of ALBP.
A
beneficial role for specific exercises or modification of posture has not been
validated by rigorous clinical studies. As a practical matter, temporary
suspension of activity known to increase mechanical stress on the spine (heavy
lifting, prolonged sitting, bending or twisting, straining at stool) may be
helpful.
Patient
education is an important part of treatment. Studies reveal that patient
satisfaction and the likelihood of follow-up increase when patients are
educated about prognosis, treatment methods, activity modifications, and
strategies to prevent future exacerbations. In one study, patients who felt
they did not receive an adequate explanation for their symptoms wanted more
diagnostic tests. Evidence for the efficacy of structured education programs
("back school") is inconclusive; in one controlled study, patients
attending back school had a shorter duration of sick leave during the initial episode
but not during subsequent episodes. Recent large, controlled, randomized
studies of back school for primary prevention of low back injury and pain have
failed to demonstrate a benefit.
Medications
used in the treatment of ALBP include NSAIDs, acetaminophen, muscle relaxants,
and opioids. NSAIDs are superior to placebo for back pain relief. Acetaminophen
is superior to placebo in the treatment of other types of pain but has not been
compared against placebo for low back pain. Muscle relaxants provide short-term
(4 to 7 days) benefit compared with placebo, but drowsiness often limits their
daytime use. The efficacy of muscle relaxants compared to NSAIDs or in
combination with NSAIDs is unclear. Opioid analgesics have not been shown to be
more effective than NSAIDs or acetaminophen for relief of ALBP or likelihood of
return to work. Short-term use of opioids in selected patients unresponsive to
or intolerant of acetaminophen or NSAIDs may be helpful. There is no evidence
to support the use of oral glucocorticoids or tricyclic antidepressants in
treatment of ALBP.
The
role of diagnostic and therapeutic nerve root blocks for patients with acute
back or neck pain remains controversial. Equivocal data suggests that epidural
steroids may occasionally produce short-term pain relief in patients with ALBP
and radiculopathy, but proof is lacking for pain relief beyond 1 month.
Epidural anesthetics, steroids, or opioids are not indicated as initial
treatment for ALBP without radiculopathy. Diagnostic selective nerve root blocks
have been advocated to determine if pain originates from a nerve root. However,
these studies may be falsely positive due to a placebo effect, in patients with
a painful lesion located distally along the peripheral nerve, or from
anesthesia of the sinuvertebral nerve. Therapeutic selective nerve root blocks
are an option after brief conservative measures fail, particularly when
temporary relief of pain may be important for patient function. Needle position
is confirmed under fluoroscopic guidance with nonionic contrast before
injection of glucocorticoid and local anesthetic.
A
short course of spinal manipulation or PT for symptomatic relief of
uncomplicated ALBP is an option. A prospective, randomized study comparing PT,
chiropractic manipulation, and education interventions for patients with ALBP
found modest trends toward benefit with both PT and chiropractic manipulation
at 1 year. Costs per year were equivalent in the PT/chiropractic group and
~$280 less for the group treated with the education booklet alone. The extent
to which this modest improvement in symptoms and outcome is worth the cost must
be determined for each patient. Extended duration of treatment or treatment of
patients with radiculopathy is of unknown value and carries potential risk. The
appropriate frequency or duration of spinal manipulation has not been addressed
adequately.
Chronic Low Back Pain
CLBP
is defined as pain lasting longer than 12 weeks. Patients with CLBP account for
50% of back pain costs. Overweight individuals appear to be at particular risk.
Other risk factors include: female gender, older age, prior history of back
pain, restricted spinal mobility, pain radiating into a leg, high levels of
psychological distress, poor self-rated health, minimal physical activity,
smoking, job dissatisfaction, and widespread pain. Combinations of these
premorbid factors have been used to predict which individuals with ALBP are
likely to develop CLBP. The initial approach to these patients is similar to
that for ALBP, and the differential diagnosis of CLBP includes most of the
conditions described in this chapter. Treatment of this heterogeneous group of
patients is directed toward the underlying cause when possible; the ultimate
goal is to restore function to the greatest extent possible.
Many
conditions that produce CLBP can be identified by the combination of
neuroimaging and electrophysiologic studies. Spine MRI or CT-myelography are
the techniques of choice but are generally not indicated within the first month
after initial evaluation in the absence of risk factors for a serious
underlying cause. Imaging studies should be performed only in circumstances
where the results are likely to influence surgical or medical treatment.
Diskography
is of questionable value in the evaluation of back pain. No additional anatomic
information is provided beyond what is available by MRI. Reproduction of the
patient's typical pain with the injection is often used as evidence that a
specific disk is the pain generator, but it is not known whether this information
has any value in selecting candidates for surgery. There is no proven role for
thermography in the assessment of radiculopathy.
The
diagnosis of nerve root injury is most secure when the history, examination,
results of imaging studies, and the EMG are concordant. The correlation between
CT and EMG for localization of nerve root injury is between 65 and 73%. Up to
one-third of asymptomatic adults have a disk protrusion detected by CT or MRI
scans. Thus, surgical intervention based solely upon radiologic findings and
pain increases the likelihood of an unsuccessful outcome.
CLBP
can be treated with a variety of conservative measures. Acute and subacute
exacerbations are managed with NSAIDs and comfort measures. There is no good
evidence to suggest that one NSAID is more effective than another. Bed rest
should not exceed 2 days. Activity tolerance is the primary goal, while pain
relief is secondary. Exercise programs can reverse type II muscle fiber atrophy
in paraspinal muscles and strengthen trunk extension. Supervised, intensive
physical exercise or "work hardening" regimens (under the guidance of
a physical therapist) have been effective in returning some patients to work,
improving walking distances, and diminishing pain. The benefit can be sustained
with home exercise regimens; compliance with the exercise regimen strongly
influences outcome. The role of manipulation, back school, or epidural steroid
injections in the treatment of CLBP is unclear. Up to 30% of "blind"
epidural steroid injections miss the epidural space even when performed by an
experienced anesthesiologist. There is no strong evidence to support the use of
acupuncture or traction in this setting. A reduction in sick leave days,
long-term health care utilization, and pension expenditures may offset the
initial expense of multidisciplinary treatment programs. In one study comparing
3 weeks of hydrotherapy versus routine ambulatory care, hydrotherapy resulted
in diminished duration and intensity of back pain, reduced analgesic drug consumption,
improved spine mobility, and improved functional score. Functional score
returned to baseline at the 9-month follow-up, but all other beneficial effects
were sustained. Percutaneous electrical nerve stimulation (PENS) has been shown
to provide significant short-term relief of CLBP, but additional studies
regarding long-term efficacy and cost are necessary.
Pain in the Neck and Shoulder
![]() Approach
to the Patient
Approach
to the Patient
In
one recent epidemiologic survey, the 6-month prevalence of disabling neck pain
was 4.6% among adults. Neck pain commonly arises from diseases of the cervical
spine and soft tissues of the neck. Neck pain arising from the cervical spine
is typically precipitated by neck movements and may be accompanied by focal
spine tenderness and limitation of motion. Pain arising from the brachial
plexus, shoulder, or peripheral nerves can be confused with cervical spine
disease, but the history and examination usually identify a more distal origin
for the pain. Cervical spine trauma, disk disease, or spondylosis may be
asymptomatic or painful and can produce a myelopathy, radiculopathy, or both.
The nerve roots most commonly affected are C7 and C6.
Trauma to the Cervical Spine
Unlike
injury to the low back, trauma to the cervical spine (fractures, subluxation)
places the spinal cord at risk for compression. Motor vehicle accidents,
violent crimes, or falls account for 87% of spinal cord injuries, which can
have devastating consequences (Chap. 369). Emergency immobilization of the neck
prior to complete assessment is mandatory to minimize further spinal cord
injury from movement of unstable cervical spine segments.
Whiplash injury is due to trauma (usually automobile accidents)
causing cervical musculoligamental sprain or strain due to hyperflexion or
hyperextension. This diagnosis should not be applied to patients with
fractures, disk herniation, head injury, or altered consciousness. One prospective
study found that 18% of patients with whiplash injury had persistent
injury-related symptoms 2 years after the car accident. Such patients were
older, had a higher incidence of inclined or rotated head position at impact,
greater intensity of initial neck and head pain, greater number of initial
symptoms, and more osteoarthritic changes on cervical spine x-rays at baseline
compared to patients who ultimately recovered. Objective data on the pathology
of neck soft tissue injuries is lacking. Patients with severe initial injury
are at increased risk for poor long-term outcome.
Cervical Disk Disease
Herniation
of a lower cervical disk is a common cause of neck, shoulder, arm, or hand
pain. Neck pain (worse with movement), stiffness, and limited range of neck
motion are common. With nerve root compression, pain may radiate into a
shoulder or arm. Extension and lateral rotation of the neck narrows the
intervertebral foramen and may reproduce radicular symptoms (Spurling's sign).
In young individuals, acute cervical nerve root compression from a ruptured
disk is often due to trauma. Subacute radiculopathy is less likely to be
related to a specific traumatic incident and may involve both disk disease and
spondylosis. Cervical disk herniations are usually posterolateral near the
lateral recess and intervertebral foramen. The usual patterns of reflex,
sensory, and motor changes that accompany specific cervical nerve root lesions
are listed in Table 16-2. When evaluating patients with suspected cervical radiculopathy
it is important to consider the following: (1) overlap in function between
adjacent nerve roots is common, (2) the anatomic pattern of pain is the most
variable of the clinical features, and (3) the distribution of symptoms and
signs may be evident in only part of the injured nerve root territory.
Table 16-2: Cervical Radiculopathy-Neurologic
Features
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Surgical
management of cervical herniated disks usually consists of an anterior approach
with diskectomy followed by anterior interbody fusion. A simple posterior
partial laminectomy with diskectomy is an alternative approach. The risk of
subsequent radiculopathy or myelopathy at cervical segments adjacent to the fusion
is 3% per year and 26% at 10 years. Although the risk is sometimes portrayed as
a late complication of cervical surgery, it may also reflect the natural
history of degenerative cervical spine disease in this subpopulation of
patients.
Cervical Spondylosis
Osteoarthritis
of the cervical spine may produce neck pain that radiates into the back of the
head, shoulders, or arms. Arthritic or other pathologic conditions of the upper
cervical spine may be the source of headaches in the posterior occipital region
(supplied by the C2-C4 nerve roots). Cervical spondylosis with osteophyte
formation in the lateral recess or hypertrophic facet joints may produce a
monoradiculopathy (Fig. 16-7). Narrowing of the spinal canal by osteophytes,
ossification of the posterior longitudinal ligament, or a large central disk
may compress the cervical spinal cord. In some patients, a combination of
radiculopathy and myelopathy occur. An electrical sensation elicited by neck
flexion and radiating down the spine from the neck (Lhermitte's symptom)
usually indicates cervical or upper thoracic (T1-T2) spinal cord involvement.
When little or no neck pain accompanies the cord compression, the diagnosis may
be confused with amyotrophic lateral sclerosis (Chap. 365), multiple sclerosis
(Chap. 371), spinal cord tumors (Chap. 368), or syringomyelia (Chap. 368). The
possibility of this treatable cervical spinal cord disease must be considered
even when the patient presents with leg complaints only. Furthermore, lumbar
radiculopathy or polyneuropathy may mask an associated cervical myelopathy. MRI
or CT-myelography can define the anatomic abnormalities, and EMG and nerve
conduction studies can quantify the severity and localize the levels of motor
nerve root injury.
Rheumatoid
arthritis (RA) (Chap. 312) of the cervical apophyseal joints results in neck
pain, stiffness, and limitation of motion. In typical cases with symmetric
inflammatory polyarthritis, the diagnosis of RA is straightforward. In advanced
RA, synovitis of the atlantoaxial joint (C1-C2; Fig. 16-2) may damage the
transverse ligament of the atlas, producing forward displacement of the atlas
on the axis (atlantoaxial subluxation). Radiologic evidence of atlantoaxial
subluxation occurs in 30% of patients with RA. Not surprisingly, the degree of
subluxation correlates with the severity of erosive disease. When subluxation
is present, careful neurologic assessment is important to identify early signs
of myelopathy. Occasional patients develop high spinal cord compression leading
to quadriparesis, respiratory insufficiency, and death. Although low back pain
is common among RA patients, the frequency of facet disease, fracture, and
spondylolisthesis is no greater than among age- and sex-matched controls with
mechanical low back pain.
Ankylosing spondylitis can cause neck pain and on occasion
atlantoaxial subluxation; when spinal cord compression is present or
threatened, surgical intervention is indicated. Herpes zoster produces neck and
posterior occipital pain in a C2-C3 distribution prior to the outbreak of
vesicles. Neoplasms metastatic to the cervical spine, infections (osteomyelitis
and epidural abscess), and metabolic bone diseases may also be the cause of
neck pain. Neck pain may also be referred from the heart in the setting of
coronary artery ischemia (cervical angina syndrome).
Thoracic Outlet
The
thoracic outlet is an anatomic region containing the first rib, the subclavian
artery and vein, the brachial plexus, the clavicle, and the lung apex. Injury
to these structures may result in posture or task-related pain around the
shoulder and supraclavicular region. There are at least three subtypes of
thoracic outlet syndrome (TOS). True neurogenic TOS results from
compression of the lower trunk of the brachial plexus by an anomalous band of
tissue connecting an elongate transverse process at C7 with the first rib.
Neurologic deficits include weakness of intrinsic muscles of the hand and
diminished sensation on the palmar aspect of the fourth and fifth digits. EMG
and nerve conduction studies confirm the diagnosis. Definitive treatment
consists of surgical division of the anomalous band compressing either the
lower trunk of the brachial plexus or ventral rami of the C8 or T1 nerve roots.
The weakness and wasting of intrinsic hand muscles typically does not improve,
but surgery halts the insidious progression of weakness. The arterial TOS
results from compression of the subclavian artery by a cervical rib; the
compression results in poststenotic dilatation of the artery and thrombus
formation. Blood pressure is reduced in the affected limb, and signs of emboli
may be present in the hand; neurologic signs are absent. Noninvasive ultrasound
techniques confirm the diagnosis. Treatment is with thrombolysis or anticoagulation
(with or without embolectomy) and surgical excision of the cervical rib
compressing the subclavian artery or vein. The disputed TOS includes a
large number of patients with chronic arm and shoulder pain of unclear cause.
The lack of sensitive and specific findings on physical examination or
laboratory markers for this condition frequently results in diagnostic
uncertainty. The role of surgery in disputed TOS is controversial; conservative
approaches often include multidisciplinary pain management. Treatment is often
unsuccessful.
Brachial Plexus and Nerves
Pain
from injury to the brachial plexus or arm peripheral nerves can occasionally be
confused with pain of cervical spine origin. Neoplastic infiltration of the
lower trunk of the brachial plexus may produce shoulder pain radiating down the
arm, numbness of the fourth and fifth fingers, and weakness of intrinsic hand
muscles innervated by the ulnar and median nerves. Postradiation fibrosis
(breast carcinoma is the most common setting) or a Pancoast tumor of the lung
(Chap. 88) may produce similar findings. A Horner's syndrome is present in
two-thirds of patients with a Pancoast tumor. Suprascapular neuropathy may
produce severe shoulder pain, weakness, and wasting of the supraspinatous and infraspinatous
muscles. Acute brachial neuritis is often confused with radiculopathy.
It consists of the acute onset of severe shoulder or scapular pain followed
over days to weeks by weakness of the proximal arm and shoulder girdle muscles
innervated by the upper or middle trunks or cords of the brachial plexus. The
onset is often preceeded by an infection or immunization. Separation of this
syndrome from cervical radiculopathy is important because slow, complete
recovery of brachial neuritis occurs in 75% of patients after 2 years and in
89% after 3 years. Occasional cases of carpal tunnel syndrome produce pain and
paresthesia extending into the forearm, arm, and shoulder resembling a C5 or C6
root lesion. Lesions of the radial or ulnar nerve can mimic a radiculopathy at
C7 or C8, respectively. EMG and nerve conduction studies can accurately
localize lesions to the nerve roots, brachial plexus, or nerves. For further
discussion of peripheral nerve disorders, see Chap. 377.
Shoulder
Pain
in the shoulder region can be difficult to separate clearly from neck pain. If
the symptoms and signs of radiculopathy are absent, then the differential
diagnosis includes mechanical shoulder pain (tendonitis, bursitis, rotator cuff
tear, dislocation, adhesive capsulitis, and cuff impingement under the
acromion) and referred pain (subdiaphragmatic irritation, angina, Pancoast
tumor). Mechanical pain is often worse at night, associated with local shoulder
tenderness, and aggravated by abduction, internal rotation, or extension of the
arm. The pain of shoulder disease may at times radiate into the arm or hand,
but the sensory, motor, and reflex changes that indicate disease of the nerve
roots, plexus, or peripheral nerves are absent.
![]() Treatment
Treatment
A
paucity of well-designed clinical trials exists for the treatment of neck pain.
Symptomatic treatment of neck pain can include the use of analgesic medications
and/or a soft cervical collar. Current indications for cervical disk surgery
are similar to those for lumbar disk surgery; because of the risk of spinal
cord injury with cervical spine disease, an aggressive approach is generally
indicated whenever spinal cord injury is threatened. Surgical management of
cervical herniated disks usually consists of an anterior approach with
diskectomy followed by anterior interbody fusion. A simple posterior partial
laminectomy with diskectomy is an acceptable alternative approach. The cumulative
risk of subsequent radiculopathy or myelopathy at cervical segments adjacent to
the fusion is approximately 3% per year and 26% per decade. Although this risk
is sometimes portrayed as a late complication of surgery, it may also reflect
the natural history of degenerative cervical spine disease. Nonprogressive
cervical radiculopathy (associated with a focal neurologic deficit) due to a
herniated cervical disk may be treated conservatively with a high rate of
success. Cervical spondylosis with bony, compressive cervical radiculopathy is
generally treated with surgical decompression to interrupt the progression of
neurologic signs. Cervical spondylotic myelopathy is typically managed with
either anterior decompression and fusion or laminectomy. Outcomes in both
surgical groups vary, but late functional deterioration occurs in 20 to 30% of
patients; a prospective, controlled study comparing different surgical
interventions is sorely needed.